Last Updated December 20th, 2021
Introduction
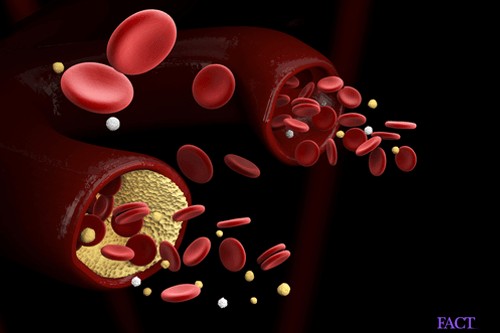
Sometimes, blood vessels can become inflamed. This condition is known as vasculitis. It causes the walls of the affected blood vessels to become thickened, making it difficult for blood to flow through normally. This condition can affect major and minor vessels in any part of the body. It can affect both arteries and veins.
What Is Phlebitis?
Phlebitis is the medical term for a condition in which a vein or a set of veins suffers from inflammation. It is also known as venitis. Veins can develop inflammation due to infection, injury or the formation of blood clots (thrombi). When blood clots are involved, this condition is referred to by the name thrombophlebitis. It can arise in any vein located in any part of the body although it tends more often to affect superficially located veins than deeper ones. The lower legs are commonly affected. Potential risks associated with thrombophlebitis in deeper veins are generally more severe as compared to more superficial cases of phlebitis. In fact, deep venous thrombophlebitis can give rise to a life-threatening condition known as pulmonary embolism.
What Causes It?
 Any condition that irritates or injures veins can give rise to inflammation in the affected veins. Causes may be intrinsic or extrinsic to the body. To give an example, an external cause could be anything that inflicts localized injury, such as the insertion of an intravenous tube. Causes intrinsic to the body itself can range from blood clots (as we have already seen) to infections or even cancer in nearby organs or tissues. Further, any condition that increases the likelihood of clot formation can also indirectly lead to phlebitis.
Any condition that irritates or injures veins can give rise to inflammation in the affected veins. Causes may be intrinsic or extrinsic to the body. To give an example, an external cause could be anything that inflicts localized injury, such as the insertion of an intravenous tube. Causes intrinsic to the body itself can range from blood clots (as we have already seen) to infections or even cancer in nearby organs or tissues. Further, any condition that increases the likelihood of clot formation can also indirectly lead to phlebitis.
The list below lays out some potential risk factors with regard to phlebitis:
- Smoking tobacco.
- Being obese.
- Taking birth control pills.
- Being pregnant.
- Prolonged periods of time spent in inactivity or leading a sedentary lifestyle can give rise to phlebitis.
- Prolonged immobility as in the case of patients who are paralyzed, hospitalized or bedridden.
- Localised injury to the vein or veins. This can occur in the form of a complication of surgery or prolonged intravenous drug use.
- Undergoing hormone therapy.
- Certain forms of cancer.
- Surgical removal of lymph nodes.
- Varicose veins.
- Bleeding disorders.
- Having a history of blood clots.
What Are The Different Types Of Phlebitis?
There are two main types of phlebitis, namely, superficial and deep phlebitis.
Superficial phlebitis: Inflammation could develop in superficial veins. In other words, it occurs in veins close to the surface of the skin. Varicose veins are distended, twisting veins that are externally visible and these, too, could develop phlebitis. Usually, there are no serious consequences associated with phlebitis in superficially located veins. The following signs could indicate a probable case of superficial phlebitis or thrombophlebitis:
- Redness along a superficial vein.
- The area may feel warm and tender to the touch.
- The vein might be swollen.
- Itching around the affected area.
- Soreness or pain.
- Hard lumps beneath the skin.
- Breakdown of skin at the affected site.
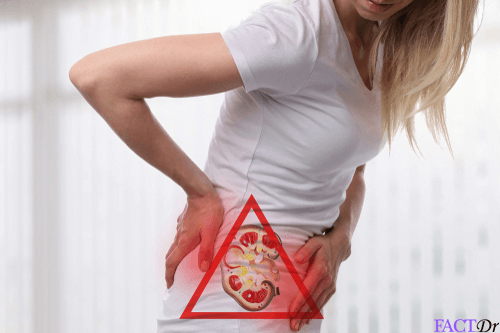
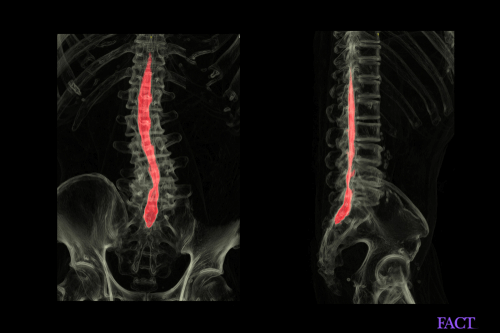
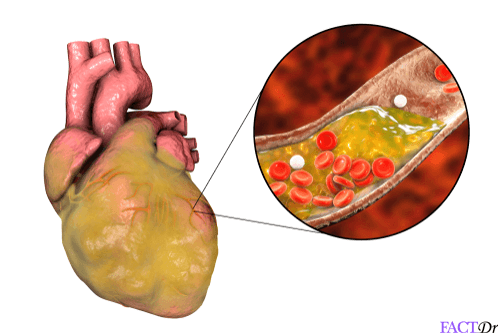
 Deep phlebitis: Sometimes a blood clot or a thrombus can form in a deeper seated vein. This condition is known as deep vein thrombosis. Such a clot can trigger inflammation in the vein. Sometimes, the problem can become compounded by infection, giving rise to a low-grade infection. Alternatively, the clot could detach and end up obstructing an artery in a lung, giving rise to a condition called pulmonary embolism.
Deep phlebitis: Sometimes a blood clot or a thrombus can form in a deeper seated vein. This condition is known as deep vein thrombosis. Such a clot can trigger inflammation in the vein. Sometimes, the problem can become compounded by infection, giving rise to a low-grade infection. Alternatively, the clot could detach and end up obstructing an artery in a lung, giving rise to a condition called pulmonary embolism.
- Lumps in the affected limb.
- Low-grade fever.
- Pain or swelling in the affected area.
- Shortness of breath, in the event of pulmonary embolism.
What Are Some Complications To Watch Out For?
A possible complication is an infection at the site of thrombophlebitis. This is known as septic thrombophlebitis and can potentially develop in instances of both superficial or deep venous thrombophlebitis. Infection could also take the form of an abscess.
Alternatively, a clot or a piece of the clot may break away and be carried along with the blood until it becomes lodged in another blood vessel elsewhere. The risk of such an outcome is greater in instances of deeper-seated thrombophlebitis. One of the more severe outcomes is a condition known as pulmonary embolism. It occurs when a blood clot becomes lodged in an artery in the lungs. When deep vein thrombophlebitis permanently damages the veins, it can give rise to a condition known as a post-phlebitic syndrome. This is characterized by chronic swelling and pain in the affected location.
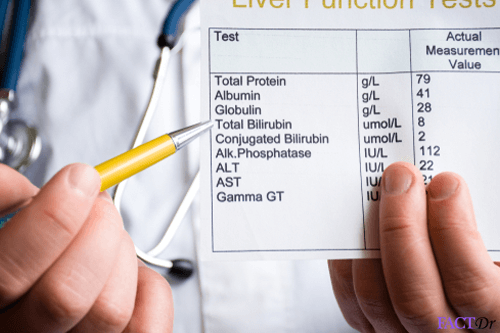
What Tests Are Needed To Diagnose It?
Phlebitis in a superficial vein is easy to recognize by means of physical examination. However, in order to make sure, the doctor must rule out other possibilities such as cellulitis (a kind of skin infection) or even insect bites that could produce similar symptoms.
- Physical examination.
- Medical history.
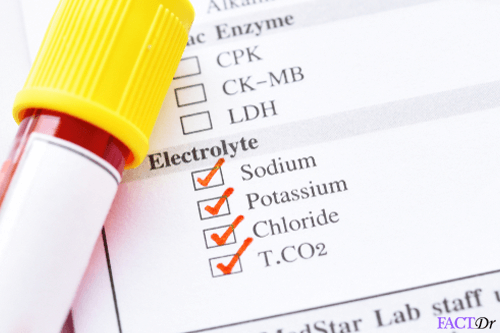
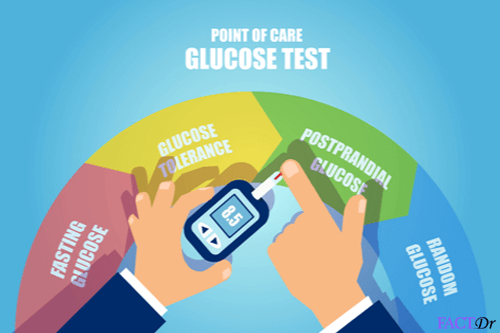
- Blood tests.
- Ultrasound imaging.
- Venography.
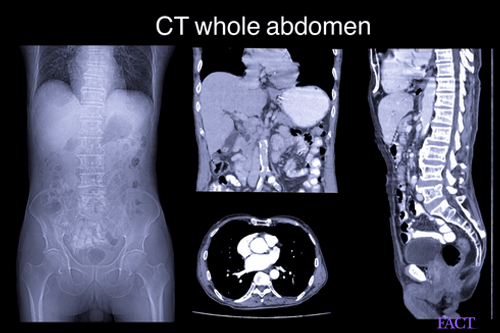
- Computerised tomography (CT) tests.
- Magnetic resonance imaging (MRI) tests.
- Skin biopsy.
- Angiography
Treatment and Prevention
 Superficial phlebitis can be treated with the help of antibiotic medications (if it is caused by a bacterial infection) and warm compresses. In case of phlebitis has resulted in DVT (deep vein thrombosis) anti-coagulants can help in preventing the formation of internal clots. For treating extensive DVT, surgery (thrombectomy) might be used. In many patients, a filter is inserted into the vena cava (major blood vessels) which will obstruct the path of any clot reaching the lungs.
Superficial phlebitis can be treated with the help of antibiotic medications (if it is caused by a bacterial infection) and warm compresses. In case of phlebitis has resulted in DVT (deep vein thrombosis) anti-coagulants can help in preventing the formation of internal clots. For treating extensive DVT, surgery (thrombectomy) might be used. In many patients, a filter is inserted into the vena cava (major blood vessels) which will obstruct the path of any clot reaching the lungs.
If one is highly likely to develop phlebitis or DVT, one should follow these precautionary measures:
- Wear compression stockings.
- Avoid long sitting and taking long flights.
- Drink adequate amount of water.
- Don’t miss out blood thinner medications.
- Don’t remain sedentary for longer durations after surgery. Start walking and moving around as soon as your doctor approves.
- https://my.clevelandclinic.org/health/diseases/17523-superficial-thrombophlebitis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1526945/
- https://www.cancer.gov/publications/dictionaries/cancer-terms/def/phlebitis
- https://bestpractice.bmj.com/topics/en-us/335/epidemiology
- https://medlineplus.gov/deepveinthrombosis.html
Dos and Don'ts
- If exercising is advised by the doctor, then the patient can engage in walking since it improves blood circulation in the lower extremities of the body.
- In case the person can’t exercise, he/she can wear compression stockings during periods of elongated sitting.
- Perform high impact exercises such as running, weight-training, squats, and lunges as it puts a strain on the calves.
- Wear uncomfortable or high-heeled shoes since these could hinder blood circulation in the legs.
Help Others Be Fit
Related Conditions
Trending Topics